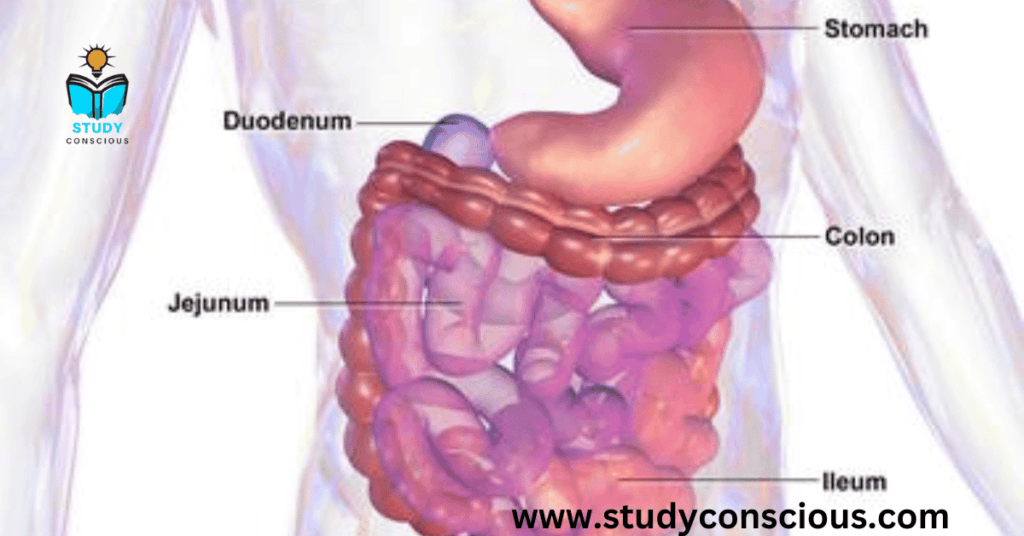
Mucositis is the painful inflammation and ulceration of the mucous membrane lining the digestive track, usually as an adverse effect of chemotherapy and radiotherapy treatment for cancer. Mucositis can occur anywhere along the gastrointestinal (GI) tract, but oral mucositis refers to the particular inflammation and ulceration that occurs in the mouth. Oral mucositis is a common and often debilitating complication of cancer treatment.
Oral and gastrointestinal (GI) mucositis affects almost all patients undergoing high-dose chemotherapy and hematopoietic stem cell transplantation (HSCT), 80% of patients with cancers of head and neck receiving radiotherapy, and a wide range of patients receiving chemotherapy. Alimentary tract mucositis increases mortality and morbidity and contributes to rising health care costs.
For most cancer treatment, about 5–15% of patients get mucositis. However, with 5-fluorouracil (5-FU), up to 40% get mucositis, and 10–15% get grade 3–4 oral mucositis. Irinotecan is associated with severe GI mucositis in over 20% of patients. Seventy-five to eighty percent of bone marrow transplantation recipients experience mucositis, of which oral mucositis is the most common and most debilitating, especially when melphalan is used. In grade 3 oral mucositis, the patient is unable to eat solid food, and in grade 4, the patient is unable to consume liquids as well.
Radiotherapy to the head and neck or to the pelvis or abdomen is associated with Grade 3 and Grade 4 oral or GI mucositis, respectively, often exceeding 50% of patients. Among patients undergoing head and neck radiotherapy, pain and decreased oral function may persist long after the conclusion of therapy. Fractionated radiation dosage increases the risk of mucositis to > 70% of patients in most trials. Oral mucositis is particularly profound and prolonged among HSCT recipients who receive total-body irradiation.
Sudden controversy about Mucositis
Why suddenly everyone stated talking about Mucositis. The medical condition suddenly came to lime light as soon as the lead TV actress Hina Khan was diagnosed with Mucositis, she was suffering from breast cancer and was undergoing treatment including sessions of chemotherapy which is the main cause behind the Mucositis. In the article we have discussed all the details about it including causes, treatment prevention, cure etc.
Signs and symptoms
Oral Cancer patients undergoing chemotherapy usually become symptomatic four to five days after beginning treatment, reaching a peak at around day 10, and then slowly improving over the course of a few weeks. Mucositis associated with radiotherapy usually appears at the end of the second week of treatment and may last for six to eight weeks.
As a result of cell death in reaction to chemo- or radio-therapy, the mucosal lining of the mouth becomes thin, may slough off and then become red, inflamed and ulcerated. The ulcers may become covered by a yellowish-white fibrin clot called a pseudo membrane. Peripheral erythema is usually present. Ulcers may range from 0.5 cm to greater than 4 cm. Oral mucositis can be severely painful. The degree of pain is usually related to the extent of the tissue damage. Pain is often described as a burning sensation accompanied by reddening. Due to pain, the patient may experience trouble speaking, eating, or even opening the mouth.[
Dysgeusia , or an alteration in taste perception, is common, especially for those who are receiving concomitant radiation therapy to the neck and mouth area. “Taste blindness”, or an altered sense of taste, is a temporary condition that occurs because of effects on taste buds that are mostly located in the tongue. Sometimes, only partial recovery of taste occurs. Common complaints are of food tasting too sweet or too bitter or of a continuous metallic taste.]
Complications
Sores or ulcerations can become infected by virus, bacteria or fungus Pain and loss of taste perception makes it more difficult to eat, which leads to weight loss. Ulcers may act as a site for local infection and a portal of entry for oral flora that, in some instances, may cause septicaemia (especially in immunosuppressed patients). Therefore, oral mucositis can be a dose-limiting condition, disrupting a patient’s optimal cancer treatment plan and consequentially decreasing their chances of survival.
Pathophysiology
There are 5 stages in Pathophysiology the 5 stages are:
- Initiation phase
- Primary damage response
- Signal amplification.
- Ulceration.
- Healing.
Diagnosis
Diagnosis is based on the symptoms the patient is experiencing and the appearance of the tissues of the mouth following chemotherapy, bone marrow transplants or radiotherapy. Red burn-like sores or ulcers throughout the mouth is enough to diagnose mucositis.
The severity of oral mucositis can be evaluated using several different assessment tools. Two of the most commonly used are the World Health Organization (WHO) Oral Toxicity score and the National Cancer Institute Common Toxicity Criteria (NCI-CTC) for Oral Mucositis. While the NCI system has separate scores for appearance (erythema and ulceration) and function (pain and ability to eat solids, liquids, or nothing by mouth), the WHO score combines both elements into a single score that grades the severity of the condition from 0 (no oral mucositis) to 4 (swallowing not possible such that patient needs supplementary nutrition). Another scale developed in 1999, the Oral Mucositis Assessment Scale (OMAS) has been shown to be highly reproducible between observers, responsive over time, and accurate in recording symptoms associated with mucositis. The OMAS provides an objective assessment of oral mucositis based on assessment of the appearance and extent of redness and ulceration in various areas of the mouth.
Prevention
A 2015 Cochrane systematic review assessing the prevention of chemotherapy-induced oral mucositis concluded that oral cryotherapy leads to large reductions in the incidence of oral mucositis of all severities in adults receiving 5-FU treatment for solid cancers. The evidence also indicates a reduction of oral mucositis in adults receiving high-dose melphalan-based cancer treatment prior to haematopoietic stem cell transplantation, although there is uncertainty regarding the size of the reduction in this instance. No evidence was found for use of this preventive measure in children. Oral cryotherapy involves the placement of rounded ice chips in the mouth, which cools the oral tissues and causes vasoconstriction. This decreases blood flow to the region and, hence, also restricts the amounts of the chemotherapy drugs delivered to the tissues.
Treatment
Mucositis will heal on its own after your course of cancer treatment has finished. If you have chemotherapy, mucositis usually appears one to two weeks after beginning treatment and heals after one to six weeks. If you have radiation therapy, mucositis appears two to three weeks after beginning treatment and heals within two to four weeks after your therapy has finished. How severe it is, and how well you take care of it to prevent additional irritation, can affect how long it takes to heal.
What should I eat or drink while healing from mucositis?
Do eat:
- High protein foods.
- Nutritional shakes.
- Soft foods.
- Sugar-free popsicles.
Don’t eat:
- Spicy foods.
- Acidic foods.
- Greasy or fried foods.
- High-sugar foods.
Do drink:
- Chamomile tea.
- Lots of water.
Don’t drink:
- Carbonated beverages.
- Alcohol.
Prevention
Can mucositis be prevented?
There’s not much in our toolbox yet to prevent mucositis from cancer treatment, but healthcare providers are working on it. Several medications are being tested that may help reduce the length and severity of the condition for certain people. Options include:
- Cryotherapy. Sucking on ice chips before and during chemotherapy treatments can help protect against oral mucositis.
- Palifermin. This drug is a synthetic version of keratinocyte growth factor (KGF), a substance your body produces to help protect and repair the cells that line your mouth and GI tract. It’s been shown to reduce the length and severity of mucositis in people with blood cancer undergoing bone marrow or stem cell transplants.
- Topical agents. Two topical gels, Gelclair® and Zilactin®, have been shown to reduce oral mucositis by coating and protecting the mucosa before radiation treatments.
- Amifostine This drug may lessen the severity of oral mucositis in people receiving radiation therapy to their head and neck when taken in advance. It may cause nausea as a side effect.